Over a span of four months in 2017, the United States experienced four deadly disasters that were likely worsened by climate change—Hurricanes Harvey, Irma, and Maria and wildfires in California.
At the time, knowledge about possible connections between climate change and cancer was limited. But after these disasters, researchers began to study how people with cancer had been affected by the events.
Today, a growing body of evidence suggests that the consequences of climate change, such as more frequent wildfires, sustained droughts and heat waves, and stronger and more intense tropical storms, may influence many aspects of cancer.
“We believe that climate change may have direct and indirect effects on the development of cancer and on cancer care,” said Gwen Collman, Ph.D., of the National Institute of Environmental Health Sciences (NIEHS), who helps coordinate NIH research on climate change and health.
For instance, climate change-related disasters can expose people to cancer-causing substances, or carcinogens, in the environment. Wildfire smoke contains several carcinogens, such as formaldehyde and benzene.
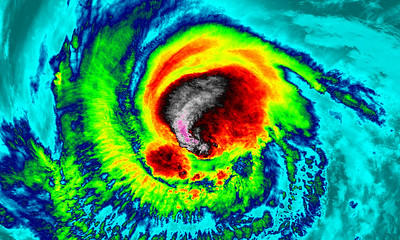
Hurricanes strengthened by warming ocean waters can destroy medical buildings and equipment used to treat, diagnose, and detect cancer. People’s access to care—and the ability of health care providers to deliver care—can be disrupted, often for long periods of time.
Extreme weather may also disrupt efforts to prevent cancer. Droughts and floods can affect the food supply, potentially reducing access to fresh fruits and vegetables. And prolonged heat waves or storms associated with climate change may discourage people from being active outdoors.
“Certainly, extreme weather events could affect the risk of cancer and efforts to prevent and control the disease in many ways,” said Curt DellaValle, Ph.D., of the Environmental Epidemiology Branch in NCI’s Division of Cancer Control and Population Sciences (DCCPS).
“Measuring and assessing these weather events will be important for understanding and addressing the impacts of climate change on health,” added Dr. DellaValle, who is a member of the NCI Climate Change and Cancer Working Group.
Connecting hurricanes and survival among people with cancer
Much of the research on climate change and cancer has focused on how hurricanes and wildfires affect cancer care.
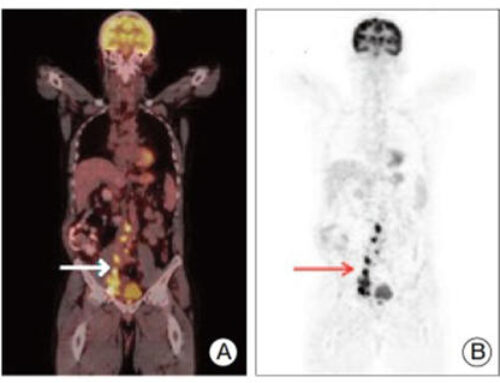
One of the first studies to measure the impact of climate change on cancer involved people who received radiation to treat lung cancer. Being treated in an area where a hurricane disaster had been declared was associated with poorer overall survival, the 2019 study found. The researchers attributed the worse survival at least in part to hurricane-related delays in treatment.
“It should not be surprising that natural disasters are going to disrupt cancer care and lead to worse outcomes for patients,” said the study’s lead investigator, Leticia Nogueira, Ph.D., a scientific director at the American Cancer Society and one of the inaugural NIH Climate and Health Scholars.
But when Dr. Nogueira proposed the study 5 years ago, her colleagues initially dismissed the idea. “Back then, few researchers were thinking about how climate change and cancer might be connected,” she recalled.
Times have changed. Dr. Nogueira now leads sessions on climate change and cancer at scientific conferences. And she is frequently contacted by cancer researchers who are interested in climate change research. Most have themselves been affected in some way by a climate-related disaster, she noted.
“A common view of climate change is that it will happen in the future and will primarily affect island nations far away,” Dr. Nogueira said. “But we are all experiencing the health consequences of climate change right here, right now.”
Listening to the voices of people affected by climate change
Stories from people with cancer who have been affected by extreme weather associated with climate change have begun to emerge. After Hurricanes Irma and Maria, researchers held focus groups with women who had been undergoing treatment for gynecologic cancers when the back-to-back storms struck Puerto Rico.
The women’s accounts of their experiences reveal the challenges they faced. Several climbed onto the roofs of their homes to try to obtain a cell phone signal to call their doctors. The calls failed, however, because nearly all of the island’s cell towers had been destroyed by the storms.
Maria dumped more rain on Puerto Rico than any storm to hit the island since 1956—an event that human-caused climate change made much more likely. Most of the women in the focus groups said their cancer treatments had been postponed or cancelled.
The women’s stories are a reminder that, although climate change affects everyone, the most vulnerable groups, including people with few resources who have diseases such as cancer, will be hit the hardest, noted Gila Neta, Ph.D., an epidemiologist with the Implementation Science Team in DCCPS.
“Communities that are marginalized tend to have a greater burden of cancer than other communities, and climate change may worsen vulnerabilities that already exist,” said Dr. Neta.
The health effects of a disaster, she noted, may persist long after that disaster has ended. A decade after Hurricane Katrina, the survival of women with breast cancer was worse among those who experienced Katrina than among those who had not been through it.
The unexpected problems of climate disasters
Extreme weather can have unpredictable and far-reaching effects for people with cancer beyond hindering access to treatment for those in the path of the storm.
For example, Hurricane Maria forced the closure of a factory in Puerto Rico that manufactured small intravenous (IV) fluid bags for hospitals. Not long after, health care facilities on the US mainland experienced a shortage of these products.
“Who would have thought that a hurricane in Puerto Rico would affect the availability of critical IV fluids for patients with cancer across the United States?” asked Robert Hiatt, M.D., Ph.D., of the UCSF Helen Diller Family Comprehensive Cancer Center, who has written about climate change and cancer.
“This example shows the complex and interconnected nature of cancer care, which is vulnerable to supply chain issues,” Dr. Hiatt continued.
He noted that the COVID-19 pandemic and major climate disasters such as Hurricane Harvey have shown “how the US health care systems are susceptible to shocks.” And, he added, “as the climate continues to change, disruptions to health care may become increasingly common.”
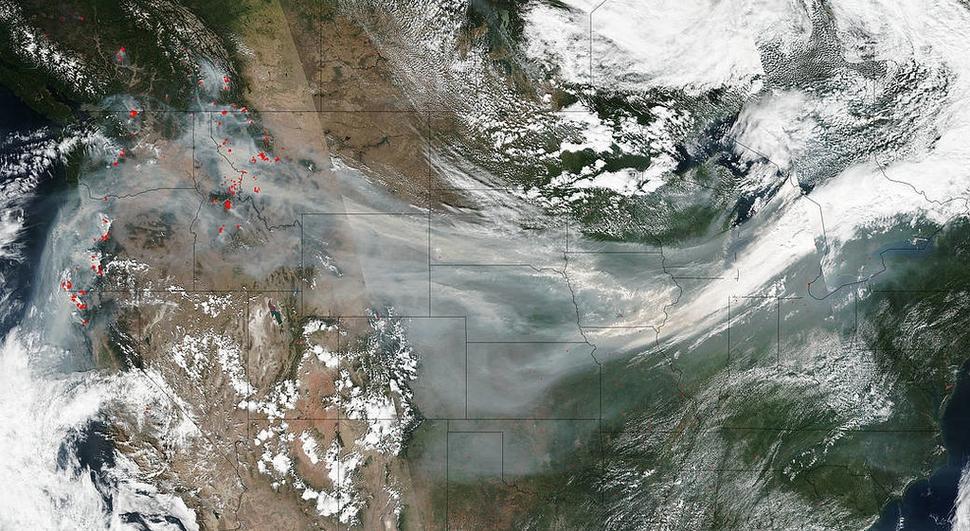
Exploring connections between wildfires and lung cancer
Dr. Hiatt became interested in climate change in part because of his experiences with wildfires in California. He was living in the San Francisco Bay Area in 2020, when smoke from these fires obscured the sun and lent the city an orange cast.
Extended droughts and heat waves associated with climate change have increased the risk and extent of large forest fires in the western United States. And one study has found that firefighters who have been exposed to smoke from these fires may have an increased risk of lung cancer.
In addition to carcinogens, wildfire smoke includes tiny particles called fine particulate matter. Exposure to these particles, which are also found in vehicle exhaust and smoke from the burning of fossil fuels, can affect the lungs and the heart.
Scientists have been exploring connections between fine particulate matter and cancer in the context of climate change. One study, for instance, has found that the global burden of lung cancer deaths attributable to fine particulate matter in the air has increased in recent decades.
Collecting data on exposures over decades
The biggest climate change-related threats for the development of cancer are likely to be from exposure to air pollution and other carcinogens, as well as disruptions to the food and water supplies, according to Dr. DellaValle.
Researchers may need to collect data on exposures over the course of a lifetime to learn how exposures to climate-related disasters affect cancer risk, Dr. DellaValle said.
Dr. Nogueira agreed. “Right now, there is a paucity of data on exposures to carcinogens released during extreme weather events,” she said. “But there is an opportunity for researchers, funding agencies, and government organizations to do better in this area.”
New technologies and approaches could help capture data on extreme weather events for health studies. For example, after a disaster, electronic questionnaires could be sent to people who were living in the affected area to collect information about their experiences, Dr. DellaValle said.
Looking to the past to understand the future
A long-running health study has recently begun to add climate change-related information to its database. The Nurses’ Health Study (NHS) is adding data on such measures as temperature, precipitation, and humidity, to each participant’s record based on the person’s zip code.
Since 1976, the NHS has collected health information from a group of nurses every 2 years. Approximately 350,000 people have been involved in the original NHS study and two subsequent NHS studies.
The expanded database could be used to explore how interactions among multiple environmental factors might affect human health, according to Jaime Hart, Sc.D., an environmental health researcher at the Harvard T.H. Chan School of Public Health and an NHS investigator.
Many previous studies, she noted, have looked at the health effects of air pollution separately from temperature and precipitation. Now, Dr. Hart and her colleagues hope to look at these types of variables together to gain insights into the complex ways that they affect human health.
“The environment is a complex system, and we’d like to look at multiple interactions,” she said.
The Nurses’ Health Study includes a team focused on cancer. These investigators plan to study such questions as whether exposure to wildfires has affected survival among people with breast or other cancers.
“We’re looking at exposures that happened up to 40 years ago, but we’re using those exposures to be able to provide information on what you may see in the future,” Dr. Hart said. “We’re on the cusp of being able to ask many new questions—stay tuned.”
A focus on emergency preparedness
For Dr. Nogueira, the challenges posed by a changing climate can be daunting. “There’s so much to do, and it can feel overwhelming at times,” she said. “But one thing that we can work on right away is emergency preparedness.”
People with cancer can prepare for emergencies by making sure they have their medications and information about their diagnoses and treatments at the ready. Online resources about emergency preparedness have information on preparing for hurricanes, extreme heat, and floods.
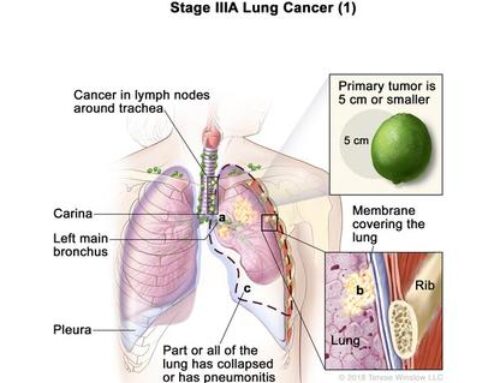
Clinicians can prepare as well. For example, based on the experience of radiation oncologists during Hurricane Maria, researchers developed modified schedules for delivering radiation therapy for various cancers during natural disasters. Radiation treatments are particularly vulnerable to disruption by disasters because electricity is needed to run the machines and water is needed to cool them.
For certain cancers, such as head and neck cancer, unplanned gaps in radiation therapy schedules may increase the chance of tumors returning, noted Hiram Gay, M.D., a radiation oncologist at Washington University School of Medicine in St. Louis. He developed the modified schedules with colleagues who have expertise in treating various types of tumors.
“Every radiation oncology clinic should have a detailed emergency-operations plan to minimize the impact that interruptions in radiation therapy have on patients,” said Dr. Gay, who experienced many hurricanes while growing up in Puerto Rico.
As the climate continues to change, more coastal hospitals may need to prepare for hurricanes. A recent study found that even relatively weak hurricanes could flood most of the hospitals in highly populated US cities on the Atlantic and Gulf Coasts.
“Climate change has raised sea levels, and higher sea levels contribute to flooding associated with hurricanes,” said study leader Aaron Bernstein, M.D., director of Harvard’s Center for Climate, Health, and the Global Environment. “And most of the research shows that climate change has already made hurricanes more intense as well.”
Hospitals in areas that have been affected by hurricanes could share lessons learned. In Miami, for example, the Sylvester Comprehensive Cancer Center has located patient care units and auxiliary generators on floors that are out of the reach of floodwaters.
Reducing health care greenhouse gas emissions
Along with emergency preparedness, reducing greenhouse gas emissions, which are a substantial contributor to climate change, is another step that health care institutions can take now.
“We don’t want to be contributing to the very problem that we’re trying to solve,” said Dr. Nogueira. Greenhouse gas emissions from the US health care system are larger than the emissions of the entire United Kingdom, she noted.
The operating room is a major driver of greenhouse gas production in hospitals, according to Anaeze Offodile II, M.D., a plastic and reconstructive surgeon at the University of Texas MD Anderson Cancer Center who has explored ways to reduce emissions at work.
“By making changes such as reducing the volume of items and instruments used just once in the operating room, we helped reduce the greenhouse gas footprint of our institution,” he said.
Other strategies for reducing emissions in health care include telemedicine. “By reducing the frequency of and distance associated with patient travel, we can make a dent in the greenhouse gas emissions footprint of health care delivery,” Dr. Offodile said.
Bringing together climate scientists and cancer researchers
Global interest in the health effects of climate change is growing. The most recent United Nations climate talks included a health pavilion that highlighted the impact of the climate crisis on the health of people around the world.
And for more than a year, the NIH Climate Change and Health Initiative has been bringing together experts to develop the knowledge that communities need to adapt and prevent further harm from climate disasters. NCI participates in this initiative.
As research on climate change and cancer advances, the knowledge gained from this work could be used to address current needs in cancer care, noted Sallie Weaver, Ph.D., of the Healthcare Delivery Research Program in DCCPS.
“For instance, finding new ways to deliver cancer care during disasters could help us make cancer care more accessible in general,” said Dr. Weaver, who manages a portfolio of research on the effects of weather-related disasters on cancer care.
Other researchers also see opportunities in the challenges presented by climate change. Dr. Collman at NIEHS points to the emergence of new scientific collaborations.
“Everyone is affected by the changes we are seeing in the climate,” Dr. Collman said. “And our research partnerships are creating connections between climate science and public health.”
She added: “We all have the same goal—to improve our ability to generate evidence and knowledge around the health effects of climate change.”

 Enlarge
Enlarge
 Enlarge
Enlarge